To hallucinate, or not to hallucinate – that is the question
The explosion of research interest, clinical development and funding of psychedelic therapeutics for disorders such as depression, PTSD and substance abuse disorder in the last decade has been both impressive and welcome.
Impressive because the scientific community has taken this by the ‘scruff of the neck’ as measured by the rapid rise of clinical trials in the field, and welcome because psychiatry is in desperate need of innovative medicines as health care systems in developed countries struggle to provide sufficient human psychotherapeutic resource to treat affective disorders.

What mechanisms drive beneficial effects of psychedelics in psychiatric disorders, and how safe are they?
The emerging consensus appears to be that drugs like psilocybin have rapid therapeutic benefit in depression and this might be driven by their psychoplastogenic effects in the cortex: essentially remodelling the cortex structure and physiology. Support for this contention comes from esketamine, which is a psychoplastogen and is approved for treatment resistant depression.
However, what is unclear is whether subjective, hallucinogenic effects of psychedelic drugs such as psilocybin are necessary for their therapeutic benefit. There is considerable evidence that agonism at the 5-HT2A receptor, a key target for psilocybin and other psychedelics, is necessary for these subjective effects. This is an important consideration if we are to deliver new treatments for psychiatry. All drugs have side effects, whether on-target or off-target driven, and it is the role of R&D to generate novel drugs with good benefit – risk profiles to gain regulatory acceptance, marketing approval, patient access, and decent commercial reimbursement.
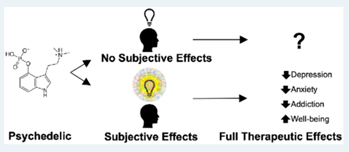 If the subjective effects of psychedelic drugs are important to their therapeutic efficacy, then there are challenges ahead on all these counts for broad indications, although for rare/orphan indications and identifiable high-risk populations they would no doubt provide immeasurable benefit.
If the subjective effects of psychedelic drugs are important to their therapeutic efficacy, then there are challenges ahead on all these counts for broad indications, although for rare/orphan indications and identifiable high-risk populations they would no doubt provide immeasurable benefit.
Psychedelics engender a range of effects, not just hallucinations
Psilocybin has both subjective and objective effects. The latter include increases in blood pressure, dilation of the pupils, anti-inflammatory effects, increases in the hormone prolactin, increase in cortical neural connections, and changes in brain connectivity and imaging. These objective measures provide opportunities to generate accurate and meaningful SAR for novel 5-HT2A ligands across multiple parameters to differentiate from existing psychedelics. Additionally, the head twitch response (HTR) and drug discrimination (DD) models in rodents are reliable in-vivo assays of 5-HT2A activity, and the potency of psychedelic drugs in these models correlates well with hallucinogenic potency in man. However, what if novel drugs activate 5-HT2A receptors but are inactive in these models – will they remain effective in depression without hallucinogenic effects? Clearly, such drugs would be desirable. But if they are inactive in our models, such as HTR or DD, how might we generate and drive SAR in a chemical series? Incorporating additional objective measures like those described above would enrich a programme. Moreover, many of these readouts also provide measurable biomarkers in man, enabling PK/PD understanding and dose-setting and facilitating clinical translation.
Can you separate therapeutically beneficial effects of psychedelics from hallucinations?
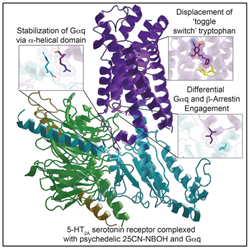
Is there a reason to believe that drugs can activate 5-HT2A receptors and not be hallucinogenic? I believe there are two compelling answers to this: Firstly, lisuride and ergotamine are 5-HT2A agonists without hallucinogenic effects in man; secondly, when a molecule activates the 5-HT2A receptor there are potentially various downstream signalling cascades that can be engaged. For the 5-HT2A receptor there is the canonical Gq/11 protein signalling cascade but there are potentially other signalling paths that are activated post ligand binding to the receptor. With the availability of ligand-docked crystal structures of the 5-HT2A receptor there is a rational structure-based approach to designing ligands that might differentially engage downstream signalling cascades. If such novel ligands are forthcoming, they might be therapeutically beneficial without hallucinogenic effects, which from a regulatory, marketing, access, pricing and real-world compliance perspective is desirable.
 This rational drug discovery approach is not necessarily limited to ligands with novel pharmacology. Today there are various biotechs/other organisations working on known psychedelic drugs and modifying pharmacokinetic, metabolic, absorptive, brain penetration/exit parameters, etc. to ascertain if there are clinical and real-world benefits relative to the original drug that might benefit psychiatric patients.
This rational drug discovery approach is not necessarily limited to ligands with novel pharmacology. Today there are various biotechs/other organisations working on known psychedelic drugs and modifying pharmacokinetic, metabolic, absorptive, brain penetration/exit parameters, etc. to ascertain if there are clinical and real-world benefits relative to the original drug that might benefit psychiatric patients.
Integrated drug discovery is key to better understanding psychedelic drug science
If we are to deliver novel 5-HT2A therapeutics to psychiatric patients, R&D programmes need a drug discovery engine that can address molecular and cellular signalling pathway understanding, consider multiple objective endpoints that could drive differentiation, and incorporate deep DMPK efforts to ensure druggability. However, costs are high, and scientific choices must be made. In all drug discovery programmes, the early lead generation phase is where exploration, generation of tools compounds and bespoke assay development should occur.
This provides a platform to drive understanding of a chemical series, leading to refinement and streamlining of a screening cascade that is fit for lead optimisation and generation of candidate molecules that can be progressed to preclinical development. This integrated approach – incorporating chemistry, bioscience, DMPK, pharmacology and preclinical development – is the core of the drug discovery engine at Sygnature Discovery.
The surge of activity in psychedelic therapeutics is leading to a deeper biological understanding of the 5-HT2A receptor, as well as other receptors these molecules engage. The biology is complex and needs unravelling, but the win is novel 5-HT2A receptor molecules with potentially broad clinical utility, spelling the introduction of innovative drugs for psychiatric patients after a dearth for decades.
We’re thinking about the science of psychedelics and ways of furthering our understanding of this important area of science using our integrated drug discovery platform. If you want to hear more about our thoughts and have a conversation, why not get in touch?
[1] Kim, Kuglae & Che, Tao & Panova, Ouliana & DiBerto, Jeffrey & Lyu, Jiankun & Krumm, Brian & Wacker, Daniel & Robertson, Michael & Seven, Alpay & Nichols, David & Shoichet, Brian & Skiniotis, Georgios & Roth, Bryan. (2020). Structure of a Hallucinogen-Activated Gq-Coupled 5-HT2A Serotonin Receptor. Cell. 182. 1574-1588.e19. 10.1016/j.cell.2020.08.024.
[2] Passie, Torsten & Seifert, Jürgen & Schneider, Udo & Emrich, Hinderk. (2002). The pharmacology of psilocybin. Addiction biology. 7. 357-64. 10.1080/1355621021000005937.
[3] Yaden, David & Griffiths, Roland. (2020). The Subjective Effects of Psychedelics Are Necessary for Their Enduring Therapeutic Effects.
[4] Olson, David. (2020). The Subjective Effects of Psychedelics May Not Be Necessary for Their Enduring Therapeutic Effects. ACS Pharmacology & Translational Science. 10.1021/acsptsci.0c00192.
[5] Thomas W. Flanagan & Charles D. Nichols (2018): Psychedelics as antiinflammatory agents, International Review of Psychiatry, DOI: 10.1080/09540261.2018.1481827
