Unravelling the Intricacies of Neuroinflammation: A Closer Look into the Brain’s Immune Response
The human brain, an amazing organ, is responsible for controlling how we feel, what we think and how we manage our bodily functions. Insulated by the blood-brain barrier, the brain was long believed to be impervious to surveillance by the immune system (so-called immune privileged)1.
Recent discoveries have revealed the presence of a complex interplay between the immune system and the brain, giving rise to the brain’s/periphery immune cell transport (glymphatic) system and the emerging field of neuroimmunology2. One key phenomenon within this field is neuroinflammation, a localized chronic immune response within the central nervous system. This blog post will delve into the growing world of neuroinflammation, exploring its causes, consequences, and implications for various neurodegenerative disorders.
What is neuroinflammation?
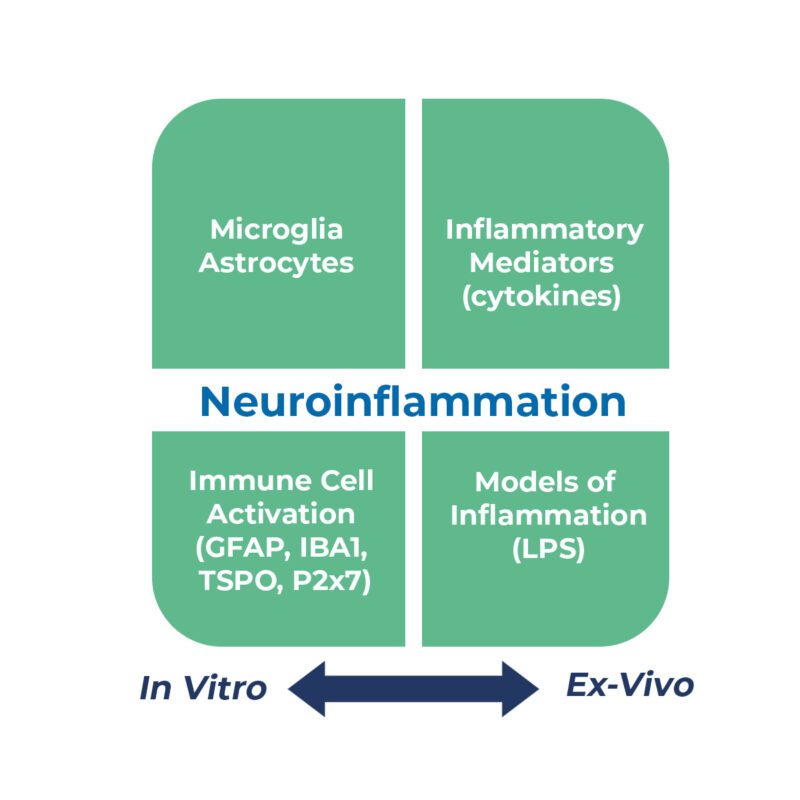
Neuroinflammation is regarded as the chronic, low-level activation of primarily resident immune cells, microglia and astrocytes, initiated by triggers like brain injury, infection, peripheral organ inflammation and chronic diseases of ageing (inflammaging, cardiovascular disease etc.)4. Key facets of neuroinflammation can be modelled in vivo by using pro-inflammatory/neurodegenerative agents like LPS, a-synuclein, b-amyloid, TDP-43 etc., and used to identify drugs with potential anti-neuroinflammatory activity.

Neuroinflammation is sustained by persistent microglia activity and the recruitment of systemic immune cells into the brain. It is a highly orchestrated process characterized by the generation of pro-inflammatory mediators, such as cytokines (e.g., IL-1, IL-6 and TNFa) and reactive oxygen species (e.g. COX-2 and iNOS5). As the most abundant immune cells in the brain, microglia are essential in protecting the brain from injury by mounting an appropriate transient inflammatory response to resolve/remove the trigger and bring the brain back to its pre-injury healthy status. However, like many innate immune cells, this process can become imbalanced such that excess production of pro-inflammatory mediators prevents the timely resolution of the initial inflammatory response6. Chronic neuroinflammation eventually leads to local tissue damage and is linked to the pathogenesis of neurodegenerative conditions, such as Alzheimer’s and Parkinson’s disease.
Neuroinflammation and Neurological Disorders
Neuroinflammation has been implicated in a range of neurological disorders, highlighting its significance in understanding the underlying mechanisms of these conditions. For example, in Alzheimer’s disease, the accumulation of beta-amyloid plaques triggers an inflammatory response, contributing to the degeneration of neurons7. Similarly, in Parkinson’s disease, inflammation has been linked to the death of dopamine-producing cells in the substantia nigra8. Researchers are actively investigating ways to modulate neuroinflammation as a potential therapeutic approach for these and other neurological disorders.
Exploring Treatment Strategies
Given the impact of neuroinflammation on neurological diseases, there is a growing interest in developing targeted anti-inflammatory treatments. Approaches to control neuroinflammation include emerging anti-inflammatory targets like NLRP39, complement inhibitors10, repurposing existing PDE4 inhibitors11, cytokine inhibitors, and immune-modulating therapies. Researchers are also exploring the potential of lifestyle interventions, such as exercise, stress reduction, and dietary changes, as adjunctive treatments to reduce long-term neuroinflammation.
Conclusion
Neuroinflammation is a vibrant area of research that has revolutionized our understanding of the brain’s immune response. Its intricate involvement in neurological disorders has highlighted the importance of considering immune-mediated mechanisms when exploring therapeutic strategies for neurodegenerative diseases. As our knowledge expands, developing novel interventions targeting neuroinflammation holds promise for improving outcomes in various neurological conditions. By unravelling the complexities of neuroinflammation, scientists are paving the way for new avenues of treatment and ultimately aiming to enhance brain health and quality of life for millions of individuals worldwide.
References
- Medawar, P. B. Immunity to Homologous Grafted Skin. III. The Fate of Skin Homographs Transplanted to the Brain, to Subcutaneous Tissue, and to the Anterior Chamber of the Eye. Br. J. Exp. Pathol. 1948, 29, 58–69.
- Kipnis, J. The Seventh Sense https://www.scientificamerican.com/article/the-seventh-sense/ (accessed Jun 19, 2023).
- Leng, F.; Hinz, R.; Gentleman, S.; et al. Neuroinflammation Is Independently Associated with Brain Network Dysfunction in Alzheimer’s Disease. Mol. Psychiatry 2023, 28, 1303–1311.
- Sun, Y.; Koyama, Y.; Shimada, S. Inflammation From Peripheral Organs to the Brain: How Does Systemic Inflammation Cause Neuroinflammation? Front. Aging Neurosci. 2022, 14, 903455.
- Tewari, D.; Sah, A. N.; Bawari, S.; et al. Role of Nitric Oxide in Neurodegeneration: Function, Regulation, and Inhibition. Curr. Neuropharmacol. 2021, 19, 114–126.
- Shao, F.; Wang, X.; Wu, H.; et al. Microglia and Neuroinflammation: Crucial Pathological Mechanisms in Traumatic Brain Injury-Induced Neurodegeneration. Front. Aging Neurosci. 2022, 14, 825086.
- Thakur, S.; Dhapola, R.; Sarma, P.; et al. Neuroinflammation in Alzheimer’s Disease: Current Progress in Molecular Signaling and Therapeutics. Inflammation 2023, 46, 1–17.
- Terkelsen, M. H.; Klaestrup, I. H.; Hvingelby, V.; et al. Neuroinflammation and Immune Changes in Prodromal Parkinson’s Disease and Other Synucleinopathies. J. Park. Dis. 12, S149–S163.
- Barczuk, J.; Siwecka, N.; Lusa, W.; et al. Targeting NLRP3-Mediated Neuroinflammation in Alzheimer’s Disease Treatment. Int. J. Mol. Sci. 2022, 23.
- Warwick, C. A.; Keyes, A. L.; Woodruff, T. M.; et al. The Complement Cascade in the Regulation of Neuroinflammation, Nociceptive Sensitization, and Pain. J. Biol. Chem. 2021, 297.
- Crocetti, L.; Floresta, G.; Cilibrizzi, A.; et al. An Overview of PDE4 Inhibitors in Clinical Trials: 2010 to Early 2022. Molecules 2022, 27, 4964.
