Crossing the Great Divide: the shadowy issue of secondary brain cancers
Dr Allan Jordan, Head of Oncology at Sygnature Discovery, shares his thoughts on this significant challenge in the field of Oncology Drug Discovery.
Primary brain tumours account for about 3% of all cancers. While these cancers start from a brain cell and remain relatively localised, many more brain cancers are secondary tumours, arising from cancer elsewhere in the body but spread into the brain.
Modern oncology drugs have had a dramatic effect on survival rates for some solid tumours such as certain types of lung, prostate and breast cancers. But as survival rates from the primary tumours improve, more people are living long enough to develop these devastating metastatic brain tumours.

1 in 3 people who die of cancer show evidence of brain metastasis at autopsy
The Great Divide
Treating brain tumours with drugs poses a significant technical challenge. Before a drug can kill cancer cells, it has to reach them, but the blood–brain barrier keeps them out. While there have been a few successes – notably Merck & Co’s temozolomide – these primarily treat brain cancer cells, and not the secondary cancers present in the brain.
And this is a huge clinical challenge. Some cancers, and it seems common in those driven by gene fusions, are more likely to form brain metastases. But the drugs that have successfully treated the primary tumour simply can’t get to them when they reappear in the brain. Data disclosed at last year’s ESMO conference in Munich suggests that about a third of all those who die of cancer have some evidence of brain metastasis at autopsy. It’s a frightening thought; are we predisposing cancer patients who believe they are being successfully treated to an unpleasant death from secondary brain tumours in a few years’ time?
There are two big failures at play here. One is that we really didn’t realise how big the problem is and has only recently become clear. But the other is that new anticancer drugs created by chemists and drug designers are not designed to pass through the blood–brain barrier. There is a compelling argument, therefore, that we should be thinking more about routinely designing oncology drugs so that they can permeate the brain.
There is, of course, also a biology conundrum. It’s not just an issue of size – some very large monoclonal antibody drugs are able to cross the blood–brain barrier, whereas many small molecules can’t. It might not just be a chemistry problem – there’s clearly some biology in play that we don’t yet fully understand but may, in time, offer novel mechanisms we can exploit.
The Path Forward
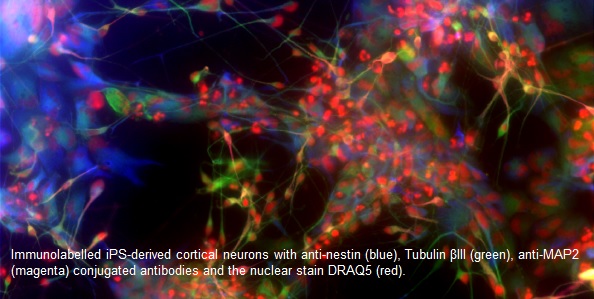
Here at Sygnature Discovery, we have a significant track record in discovering drugs that work on the central nervous system, and we understand the properties that molecules need to have if they are to get into the brain. Our colleagues at RenaSci, a Sygnature Group company, have a huge amount of expertise in assessing brain permeability. The same techniques and thought processes can easily be applied to anticancer drug discovery programmes.
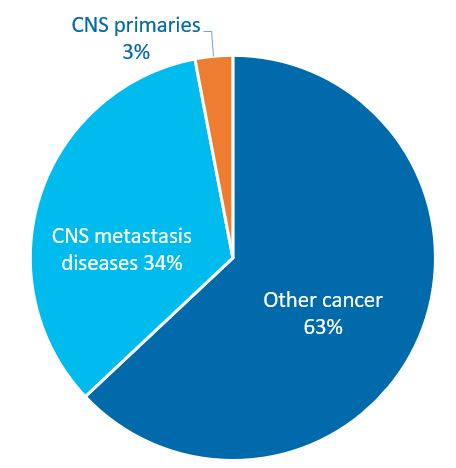
Whilst only 3% of cancer patients suffer primary brain cancers, a third will die with their primary cancer having spread into the brain.
There are already promising examples of cancer drugs for non-CNS cancers that can also get into the brain, such as LOXO’s kinase inhibitor larotrectinib (trade name Vitrakvi™), which treats solid tumours that are driven by NTRK gene fusions. Kinase inhibitor drugs are rarely able to cross the blood–brain barrier, but larotrectinib is a significant exception – it has phenomenal activity in CNS metastatic disease. So, it’s not impossible. Is there really any reason why we shouldn’t expect to do this every time?
We need to strive to incorporate the right properties into the molecule at the outset, while avoiding wherever possible those attributes that stop it getting into the brain. If we can do this routinely, then perhaps the prospects for patients with brain metastases might be less bleak. We believe it’s time for us to work together to deliver the next generation of effective, safe and well-tolerated oncology drugs that also work on tumours in the brain, regardless of mechanism of action. The challenges will not be insignificant. But the lives of over 3 million people are a powerful argument for a determined effort.
We continually engage with our industry on a range of drug discovery topics. If would like to discuss oncology drug discovery, our capabilities or even drug discovery in general then we’d love to hear from you. You can get in touch by using any of the contact forms.
