Substance Use Disorders: Identifying new Treatments for Opioid Abuse
Adulteration of opioids with fentanyl and nitazenes has, in part, been responsible for the huge increase in drug related deaths in the USA and Canada. These synthetic opioids can be 1000’s of times more potent than morphine, meaning very small quantities can be illegally imported for adulteration of drugs such as heroin. Their high potency can result in opioid toxicity which is not easily reversed with opioid antagonists such as naloxone. The presence of synthetic opioids is not unique to the USA. Recently nitazenes have been detected in heroin in the UK and Australia.
Reducing reliance on illicit drugs is a practical method of reducing deaths of people with substance use disorders. Doctors have prescribed safer opioid agonists and partial agonists for decades as maintenance therapy. These drugs, such as methadone and buprenorphine, reduce cravings for opiates without producing the euphoric high and risks associated with illicit opiates. However, maintenance programs are not without drawbacks. It is estimated that up to 57% of patients relapse to heroin within 6 months of tapering off methadone. Therefore, there is still a need for safer and more efficacious opioid maintenance therapies.
To assess the efficacy of novel opioid maintenance therapies, preclinical abuse liability models can be repurposed. In particular, the intravenous self-administration and physical dependence models are reliable models for evaluating drug seeking and withdrawal symptoms engendered by drugs of abuse.
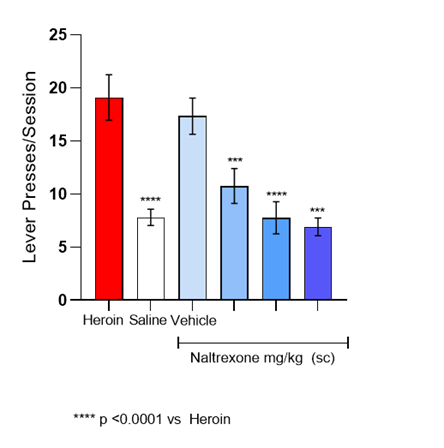
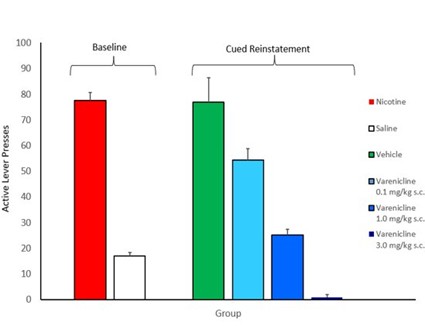
The intravenous self-administration model involves training rats to self-administer addictive drugs in operant boxes. By administering novel putative therapeutics prior to operant training sessions, it is possible to evaluate whether a compound reduces motivation to consume the drug of abuse. Current medications for substance use disorder are reliably effective in this model. For example, naltrexone reduces heroin consumption and varenicline reduces nicotine seeking in this model (see Figures below).
The physical dependence model involves inducing dependence to an addictive drug. As with people that chronically administer drugs, dependence develops over time and when the drug is no longer available characteristic withdrawal symptoms are produced. Novel therapies can be evaluated for their propensity to reduce withdrawal symptoms by substituting the drug of abuse with the test compound. Therapies such as methadone reliably reduce withdrawal symptoms associated with chronic morphine administration.
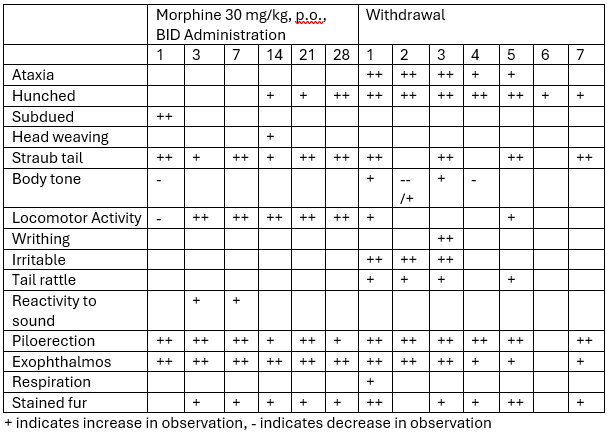
Sygnature Discovery has evaluated two novel compounds for use as opioid maintenance therapies in the physical dependence model.
